Must Know
These are salient points you MUST know
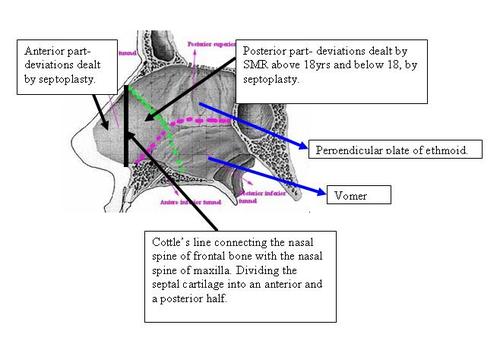
What are the parts of the nasal septum
The nasal septum comprises of an anterior cartilaginous and posterior bony part. The bony part behind comprises of the perpendicular plate of ethmoid above and the vomer below.
Surgery for Nsal septal deviations:
Anterior septal cartilaginous deviations are dealt with septoplasty and posterior septal cartilaginous are dealt by septoplsty ,if less than 18 years...since the posterior cartilaginous septum contains a growth center that contiues to grow till the age of 18years..hence if this is resected below this age, it will lead to developmental hypoplasia of the entire mid third of the face. Above the age of 18 years, the posterior cartilaginous septum can safely be resected and hence therfore SMR is performed.
Complicaions of SMR
If the dorsal strut is not retained, there can be dorsal saddling.
If the caudal strut is not retained, there can be columella reraction.
Jointly, if both are present , the nose will look like the beak of a parrot, Poly beak deformity.
If blood accumulates between the two flaps, then, Septal haematoma.
If this gets infected, then, septal abscess.
This will lead to avascular necrosis of flaps, resulting in septal perforation.
Adenoid facies
· Adenoid facies: It is generally accepted that a child with enlarged adenoids has a characteristic facial appearance resulting from effect of nasal obstruction and mouth breathing on the growth of maxilla. This facial appearance consists of:Complications of Tonsillectomy:
Primary Haemorrhage- on the table during the surgery
Reactionary haemorrhage- between 4-6 hours..due to either rebound hypertension after the anaesthetic effect wears off or due to slipping of the ligature.
Secondary haemorrhage- between 6-10 days, due to the slough in the tonsillar bed getting infected. This happens if the child is not encouraged to chew in the postop days. This child may not chew due to fear of pain, and if so, the slough in the tonsillar bed will not get seperated by muscle contraction...and this slough can get infected resulting in secondary haemorrahage.
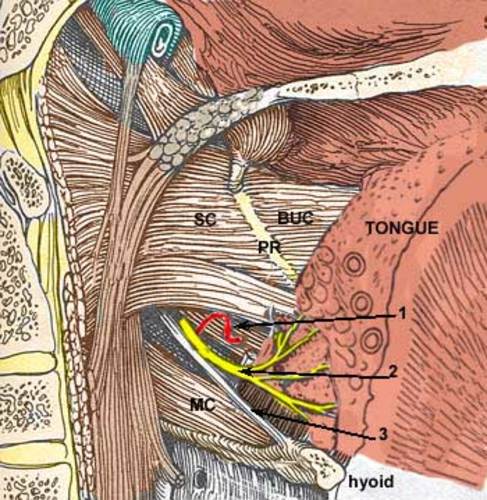
Tonsillar Bed:
What is the Cottles line:
Its an imaginary vertical line drwan from the spine of frontal bone above to the spine of maxilla below-dividng thecartilaginous septum into an anterior and posterior part.
The anterior part is essential to maintain the integrity of the architecture of the external nose and therefore cannot be resected.
The Cottle test is useful to evaluate nasal valve stenosis. The cheek of the evaluated side is gently pulled laterally with 1-2 fingers, which opens the valve. The examiner then asks the patient to breathe and evaluates if breathing is better before or after pulling the cheek. A positive test result is when the patient feels less resistance with the valve opened. This test is easy and quick to perform (see the image below).
Sequence in the management of sinus disease
First a broad spectrum antibiotic is given with a mucolytic.
If the patient does not respond, a proof puncture is performed.
Next antral lavage is performed.
If the disease persists, Intra nasal antrostomy is done- INA
Still if the disease persists, Caldwell Luc operation is done.
Today we know that the antrum does NOT drain by gravity and therefore, the natural ositum is opened by performing
functional endoscopic sinus surgery is done wherein the natural ostium in the middle meatus is widened by
Endoscopic middle meatal antrostomy.
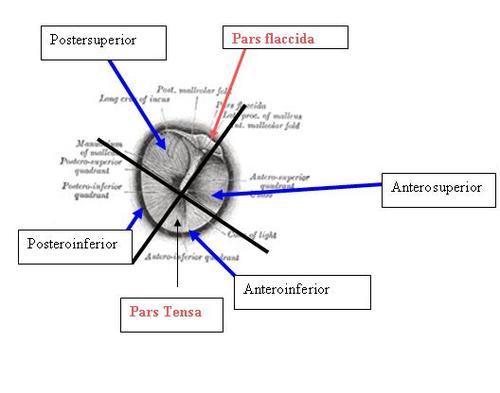
Describe and name the parts and divisions of the tympanic membrane
The tympanic membrane is divided into an upper pars flaccida and a lower pars tensa.Pars flaccida is so since it lacks the middle fibrous layer and therefore flaccid. The lower pars tensa consists of all three layers, namely the outer epithelial layer, the middle fibrous layer and the inner mucous layer.
The annulus fibrosus tympanicus is the thickened peripheral rim of the pars tensa of the tympanic membrane. It is an area into which the connective tissue matrix of the tympanic membrane extends to attach to the tympanic bone (ring).
The tympanic membrane is divided into 4 quadrants by two imaginary lines - one drawn along th handle of the malleus and another imaginary line at right angles to the first line at the umbo. By this we have therfore, anterosuperior, anteroinferior, posterosuperior and posteroinferior quadrants.
Central Perforation
A central perforation of the tympanic membrane is one in which the perforation is surrounded on all sides by a remnant of the tympanic membrane. Here the annulus fibrosis is intact. This is also called a safe ear. Called safe because the life threatening complications of the unsafe variety does not occur. Explanation: In a safe ear, the annulus is intact. The annulus acts as a barrier preventing the inward migration of outer canal wall skin into the middle ear- if it happens, its called, skin in the wrong place, also called cholesteatoma.
In a safe ear, the perforation of the pars tensa is surrounded by a remnant of tympanic membrane.
Marginal perforation:
A marginal perforation of the tympanic membrane is one in which the perforation adjoins the bare bone of the cananl wall- the anulus is eroded...thereby permitting easy migration of the outer canal wall epithelium into the middle ear resulting in cholesteatom which can cause life threatening complications.
Stages of tubotympanic disease:
Active: wherein the ear is actively discharging
Inactive: Dry perforation of the ear drum. Intact annulus. Normal middle ear mucosa.
Quiescent stage : Discharege stopped just a few days back.Middle ear mucosa maybe normal or hypertrophied.Central perforation present.
Healed : healing of the drum by a thin monolayer.Intact ossicular chain.
Workup of a Ear case:
Examination under microscope
Culture and sensitivity if there is discharge
Patch test
Pure tone audiometry
Eustachiantube evaluation
Mastoid xray
Reasons for taking mastoid xray
- To know the extent of mastoid pneumatisation
- TO know if there is a forward lying sigmoid sinus or a low lying dura
- To know the existence of a korners septum: if the korners septum is not detected, then deeper diseased cells maybe left behind during cortical mastoidectomy resulting in residual disease.
Körner's septum (petrosquamosal lamina)
bony septum separating the mastoid antrum from the aerated cells in the squamous part of the temporal bone. Erosion of this septum may be seen in cholesteatoma extending from the middle ear towards the mastoid antrum

D-Korners septum
Complications of CSOM
Intracranial
Surgical options for a ear case:
- Safe dry ear where the patch test reveals recovery of hearing-Myringoplasty
- Safe dry ear with conductive loss...inadequate recovery--suggestive of ossicular damage-ossiculoplasty with tympanoplasty
- Discharging safe ear not responding to appropriate medical therapy: Cortical mastoidectomy with tympanoplasty
- Unsafe ear with moderate hearing loss--modified radical mastoidectomy with cavity obliteration and tympanoplasty
- Unsafe ear with severe conductive hearing loss- radical mastoidectomy
- Safe ear DRY -patient not willing for surgery but wants perforation closure- kartusch tympanic membrane patcher.
- Safe ear, dry-patient does not want any procedure but wants hearing-hearing aid.
- Safe ear discharging periodically,surgical risk..patient wants hearing-bone anchored hearing aid.
Workup of a nose case:
Nasal discharge for culture sensitivity
Diagnostic nasal endoscopy
Plain exray waters view for maxillary sinus and caldwell view for frontal sinus. The spenoid sinus is visualised by open wouthed waters view...through the open mouth.
Dangerous area of face:
Dangerous area of face:
Dangerous area of face comprises of upper lip,lower part of nose and adjacent area. This area has been so named because boils, infections of the nose and injuries around the nose, especially those that become infected can readily spread to cavernous sinus resulting in cavernous sinus thrombosis (CST). CST is generally a fulminant process with high rates of morbidity and mortality. Fortunately, the incidence of CST has been decreased greatly with the advent of effective antimicrobial agents.
Anatomical Considerations:Anterior facial vein begins at the side of root of nose through the union of supra-orbital and frontal veins. The vein drains upper lip, septum of nose and adjacent areas. The anterior facial vein communicates with the cavernous sinus through the ophthalmic veins. It also communicates with cavernous sinus via deep facial vein which connects the pterygoid plexus with anterior facial vein.
Key points: Anterior facial vein has no valves and it makes possible bidirectional blood flow in the vein. It lies amongst muscles which by contraction may displace the clot in the vein. This area (dangerous area of face) is lacking in deep fascia, which acts as barrier to the spread of inflammation and the infective processes have ready access to muscles. The highly anastomotic and valve less venous system allows retrograde spread of infection to the cavernous sinus via the superior and inferior ophthalmic veins. Any forceful squeezing, manipulation of furuncle, infection or abscesses in this area may push up the infection towards the cavernous sinus. Nasal septal abscesses that may follow trauma or surgery should be carefully incised avoiding any injury to the adjoining healthy area. If the healthy tissue is incised in the neighborhood of infection, the infection may reach the veins and result in clot formation. This clot in turn may be pushed up through the valve less veins by movements of the facial muscles to the cavernous sinus. The adequate management of facial furuncle to prevent spread of infection to cavernous sinus is of paramount importance. Staphylococcal infection of a hair follicle is the usual cause. A furuncle is a deep seated, firm, tender nodule that enlarges, becomes erythematous, painful and fluctuant after several days. This localized infection, may develop into an abscess. The treatment comprises moist heat initially; most strains of staphylococci are sensitive to clindamycin and doxycycline. Surgical incision and drainage is required when fluctuation is palpable. Systemic treatment with antibiotics is indicated for systemic symptoms or extensive cellulites. Cavernous Sinus Thrombosis is characterized by severe headaches, neck stiffness, altered consciousness levels and epileptic fits. Clinically there is high grade fever, rigors, headaches, a reduced conscious level, and signs of cerebral irritation. An ophthalmoplegia results from paralysis of cranial nerves that travel within CS viz III, IV and VI and ophthalmic and maxillary nerves. The eyes are proptosed with considerable swelling in the area. The mainstay of therapy is early and aggressive antibiotic administration. Although S aureus is the usual cause, broad-spectrum coverage for gram-positive, gram-negative, and anaerobic organisms should be instituted pending the outcome of cultures. IV antibiotics are recommended for a minimum of 3-4 weeks.
Techniques of Myringoplasty:
Overlay: after clearing the outer epithelial layer, the graft is placed on the drum remnant
Underlay technique: The graft is placed underneath the drum remnant after scrapping clear the undersurface mucosa..here there is the risk of mucosa from the lateral border growing medially , above the graft, gaining access through the perforation to the outer surface of the drum and causing persistent mucositis.
To avoid this:
Interlay technique: Here the graft is placed on the bare bone of the outer canal wall , thereby prempting the possibility of mucositis. This is done by elevating a tympanomeatal flap, including the drum remnant, and placing the graft on the bare bone..ie, between the middle fibrous layer of the drum remnant and the inner mucous layer of the middle ear...the interlay technique.
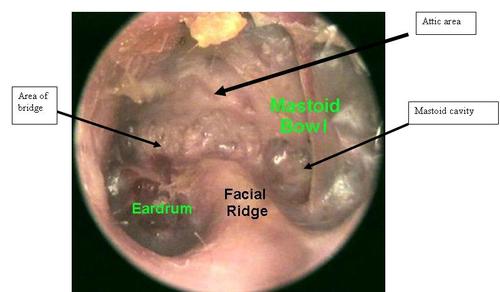
Mastoid surgeries:
Cortical mastoidectomy is performed to exenterate all diseased mastoid air cells when a discharging ear is not responding to adequate medical therapy.
Modified Radical Mastoidectomy is performed for an unsafe ear. The goal of modified radical mastoidectomy is to exenterate the disaease and to create a perfectly exteriorised cavity that can periodically inspected and cleaned. The disadvantage is that there is a residual cavity.
The difference between modified radical mastoidectomy and cortical mastoidectomy is: in MRM, the bridge is removed and the ridge is lowered. The bridge is the connecting ledge of bone that bridges the notch of rivinus--this has to be removed to gain access to the attic area. The Ridge is the deep posterior meatal wall that deeper in houses the facial nerve is sufficiently lowered such that the cavity can perodically be inspected from the external ear for cleaning. If the ridge is not sufficiently lowered, then there will be a sump in which debri can accumulate. The healthy ossicular chain is retained.
In order to avoid the cavity , today we can perform, modified radical masotidectomy, mastoid cavity obliteration, ossicular reconstruction, and tympanoplasty in order to give the patient a reconstructed servicable ear.
Head Mirror:
1858
- Czermak presents his successful findings to the Viennese medical community and is catapulted into history as the inventor of the head mirror.
Standard size 9 cm dia. with 1.3 cm aperture.
Throat Case:


Exam of oral cavity here:
http://www.encyclopedia.com/video/IXQJWXJi9g0-14oral-cavity-examavi.aspx
Examine the lips, angle of mouth, vestibule of mouth, buccal mucosa, gingiva, tooth, dorsal ventral surface and lateral borders of tongue, floor of mouth and hard palate in the oral cavity and anterior pillar tonsil, soft palate, uvula, posterior pharyngeal and base of tongue in the oropharynx. Next, indirect larngoscopy is performed using indirect laryngoscopic mirror. The examination is compete by performing the postnasal examnation and lastly examination of the neck.
Pearls:
- If hearing loss on puretone audiometry exceeds 60db, ossicular chain disruption should be suspected.
- Rose position in tonsillectomy is flexion of the neck and extension of the atlantooccipital joint.
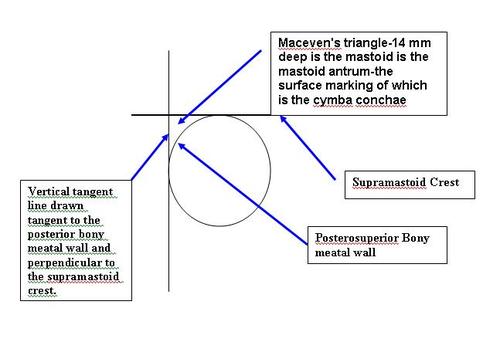
Macevans Triangle
Suprameatal trianngle:
In the temporal bone, between the posterior wall of the external acoustic meatus and the posterior root of the zygomatic process is the area called the suprameatal triangle, mastoid fossa, foveola suprameatica, or Macewen's triangle, through which an instrument may be pushed into the mastoid antrum.
In the adult, the antrum lies approximately 1cm deep to the suprameatal triangle. This is an important landmark when performing a cortical mastoidectomy. The supreameatal triangle lies deep to the cymba conchae.
Sir William Macewen, CB, FRS, (22 June 1848 – 22 March 1924) was a Scottish surgeon. He was a pioneer in modern brain surgery and contributed to the development of bone graft surgery, the surgical treatment of hernia and of pneumonectomy (removal of the lungs).
Further details at:
http://en.wikipedia.org/wiki/William_Macewen